Books Reviewed
Decades ago, during my first week of anesthesiology training, a professor advised me to give a drying agent to black patients if they needed to have a breathing tube inserted while awake. In my professor’s experience these patients produced more oral secretions during airway instrumentation, which complicated the procedure. Later in my training, another professor told me that I should lower the dose when administering narcotics to my Asian patients, because they were more sensitive to that family of drugs.
The first of these professors was Jewish and gay, and so did not fit the stereotypical racist profile; the second was one of the most famous anesthesiologists in the world. Neither one of them was either racist or stupid. Yet when I mentioned their recommendations in print years later, critics did call them both racist and stupid, with some of the bad odor clinging to me for having cited them. Since then I have learned, as most doctors have, that it is okay to talk about diseases associated with certain ethnic groups—for example, Tay-Sachs disease in Ashkenazi Jews or sickle cell anemia in blacks—but not to make isolated ethnic-based or gender-based clinical observations, even if the goal is to prompt more clarification through testing. (For example, it has now been shown that Asian sensitivity to narcotics is nothing more than a weight-dependent phenomenon.)
This has been the extent of my personal contact with political correctness in medicine. But more is out there. In 2002 Dr. Sally Satel, a resident scholar at the American Enterprise Institute, published her book PC, M.D., which highlighted a trend of increasingly restrictive speech codes in psychiatry. Last year, Dr. Gary Tigges was forced to resign from his hospital leadership post in Texas when he blamed the gender pay gap among physicians on the fact that female doctors “do not work as hard.” He was wrong—doctors of both genders work equally hard. But what he was trying to say, somewhat artlessly, was that female doctors work fewer unit hours on average than male doctors do. That point was later substantiated by a study in the Journal of the American Medical Association.
* * *
None of these examples exposes political correctness at medicine’s scientific core, where non-psychiatric diagnoses and treatment plans are formulated. For that we have Dr. Theodore Dalrymple’s new book, False Positive: A Year of Error, Omission, and Political Correctness in the New England Journal of Medicine. Rather than pluck the most scandalous examples of political correctness from whatever time and place he might find them, Dalrymple has scrutinized a year’s worth of weekly issues from the New England Journal of Medicine (NEJM), America’s flagship medical journal, over the course of 2017. By combing systematically through a widely respected publication, he has ensured that his results are more than anecdotal.
Dr. Dalrymple is one of the best and most engaging physician writers around. In False Positive, he covers a wide range of topics, devoting a short chapter to each issue of the NEJM.
Still, an overarching narrative is lacking. The reader wonders where this week-by-week analysis is headed and what conclusions might be drawn. When Dalrymple does undertake to summarize things, he describes all of the shortcomings he has found in the NEJM as political correctness. But that description ties together too many things that may not deserve to be tied together. As I read the book, it seemed to me as if only some of the NEJM’s transgressions were truly motivated by political correctness as most people understand the term (that is, by willful enforcement of race- or gender-based pieties). Other infractions boiled down to arrogant science, and still others to a conflation of association and causation.
* * *
In fact, when it came to political correctness, the NEJM furnished only a few really outrageous examples. One article made charges of “institutional racism” against U.S. health authorities, because the mortality rate for hepatitis C infection is greater for American Indians than for whites. Yet an institution is a thing, and a thing cannot be racist. Since institutions are composed of people, the charge of “institutional racism” is really a cover for charging the people who make up an institution with racism.
This is infuriating. It suggests that doctors and nurses working in the U.S. government take less interest in cases of hepatitis C among American Indians than in those among whites. It is similar to the claim that American doctors are racist because black women suffer higher morbidity and mortality rates while giving birth than white women do. I practiced obstetrical anesthesia for 30 years in a hospital that served a large population of African Americans from the inner city. I observed a higher rate of complications among these women because of their dramatically increased incidence of morbid obesity, which makes childbirth very dangerous, as well as their high rate of failure in keeping their pre-natal care appointments. The insinuation that white doctors and nurses are a bunch of racists who don’t work as hard on behalf of pregnant African-American women (or American Indians suffering from hepatitis C) is a damn lie.
Other examples of political correctness in the NEJM consisted more of silly virtue signaling than of outright finger-pointing. Dalrymple catches one author describing an experiment with “female and male mice” as opposed to the more common phrase, “male and female mice.” One can imagine the study’s author thinking about this diction for days, titillated by the thought of scoring a point against the patriarchy. Such pettiness has serious social ramifications when several hundred million people indulge in it. But in terms of health policy, it’s harmless.
* * *
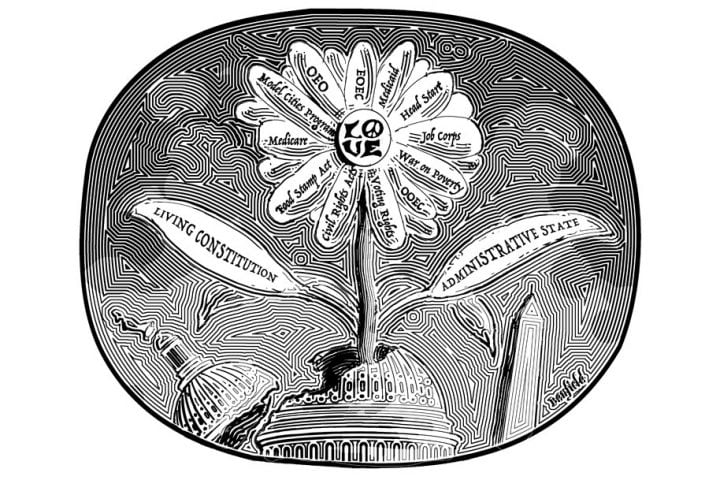
There are other phenomena covered by Dalrymple’s book for which political correctness may not be the best explanation. For example, one NEJM article expressed dejection over the fact that rich people are healthier than poor people. Dalrymple sharply observes that the words injustice and inequity are nowhere used when rich people suffer more diseases, implying that “no injustice can be done to the rich, or that justice is not due to them because they are rich.” Yet this obsession with equity long predates the era of political correctness. Alexis de Tocqueville commented on the same phenomenon almost 200 years ago.
I myself witnessed this obsession play out in academic medicine while attending a public health conference shortly before the Affordable Care Act was passed in 2010. I listened to several professors denounce with practically molten rage their favorite example of inequity, which they had dedicated their lives to fixing. Later, I spoke with two of the public health economists responsible for crafting Obamacare. They poked fun at certain health policy journals I follow, such as Health Affairs, for what they called amateur economic modeling. Although one hopes Obamacare’s disastrous rollout taught these two some humility, none of this is modern-day political correctness. A quote from Theodore Roosevelt over a century ago, “Envy and arrogance are the two opposite sides of the same black crystal,” sufficiently captures the conference’s spirit.
According to Dalrymple, another result of political correctness is the NEJM’s tendency to sanitize language. For example, when talking about medically assisted dying, one NEJM author used the word intervention to describe a doctor giving a patient the means to kill himself. Yet such phraseology may have motivations other than political correctness. True, political correctness favors euphemism—as, for example, when fat people are called “weight-challenged.” But euphemism can also be used to describe something unpleasant in softer terms. The act of killing oneself is certainly unpleasant.
In addition, some speakers substitute Latinisms for dull Saxon words, to sound smart. The NEJM author who substituted the word “intervention” for the phrase “help to kill” may have been doing just this.
The authors Dalrymple criticizes may or may not know that their narrow three-page investigations, guided by the scientific method and written in scientific language, cannot solve intractable human problems—such as drug abuse, depression, or terminal illness—in which thousands of independent variables are involved and no two people are exactly alike. Maybe these authors are vain and need fancy words to protect their vanity. Then again, maybe they really believe life’s most profound questions have straightforward scientific answers if couched in fancy language. In which case they are just fools.
* * *
Dalrymple is at his best when wrestling with such thorny medical issues, which ultimately have no obvious right or wrong answer. He offers the wise discussion that we wish we found in the NEJM instead of verbal preening. But verbal preening is not political correctness. In fact, in some cases, it may even constitute resistance to political correctness, a kind of windbreak against the hyper-subjectivity and emotionalism of progressive shibboleths.
Other NEJM missteps in False Positive involve the mistaken tendency to assume that factors associated with a given event must necessarily have caused that event. Dalrymple notes how one study’s authors, having observed an association between air pollution and rising death rates, leapt to the conclusion that air pollution causes high death rates. The fact that air pollution is worse in areas where other unhealthy things exist undermines that conclusion. Errors of this type have become so common as to represent modern-day mass superstitions. But we might expect doctors writing for the NEJM to be above such madness.
Readers of Dr. Dalrymple’s book will learn the limits of the scientific method and the difference between association and causation. Indeed, he says he embarked on the project to show his nephew how to read a medical research paper critically. False Positive accomplishes this goal, and should be required reading for every medical doctor and nurse in training. But on the subject of political correctness, it doesn’t really advance the debate.